As February is Fowler’s Syndrome Awareness Month, I decided to find out what some common questions were that people have about Fowler’s, as well as asking others with the diagnosis what they wish they had asked when it was first brought up for them. One of the things I’ve been asked the most is ‘what is your fowlers story?’ but I’ve decided to leave this for a separate post for now as it’s pretty long!
What are the main symptoms and what were your initial symptoms?
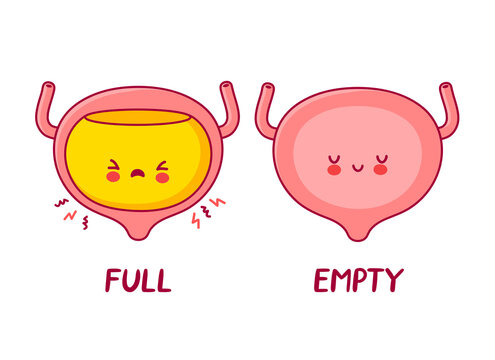
The main symptom is an inability to urinate – this can either be a partial inability or full inability. Sometimes people may have to strain to empty their bladder, or take a long time to fully empty their bladder. Bladder spasms can be a huge issue for people with the condition as well.
Often, people are unable to feel when their bladder is full. I rarely have bladder sensation unless I have an infection (which is when I often feel like I constantly need to go to the toilet).
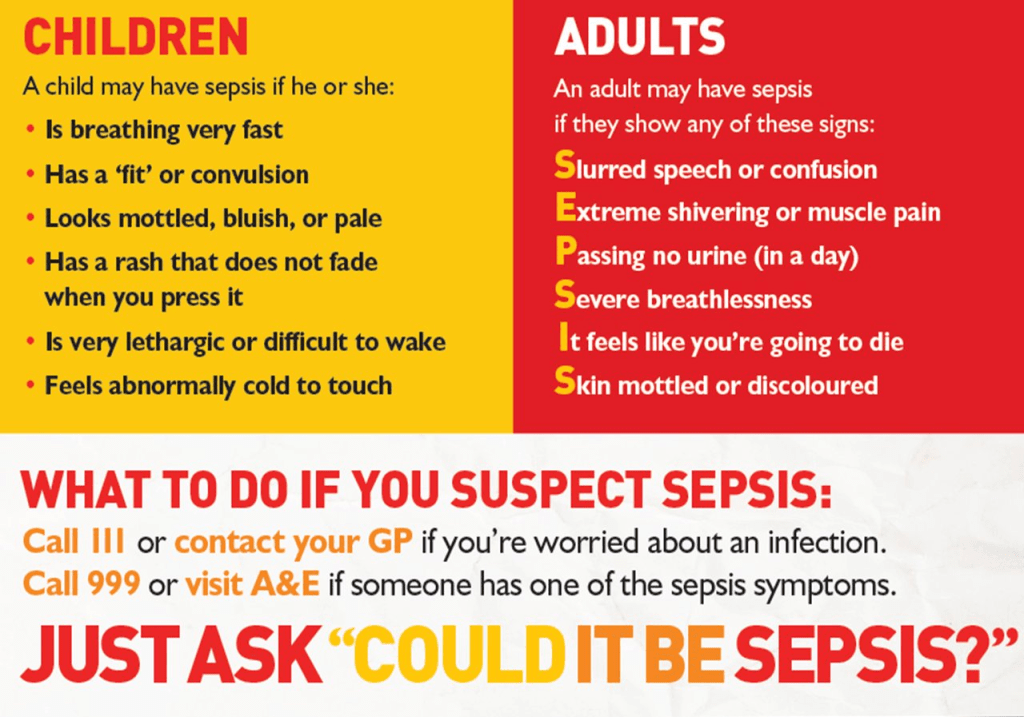
Stomach, bladder and pelvic pain are common side effects of Fowler’s. Pain can increase with specific movements and activities. Frequent infections can also exacerbate pain levels. Infection is also common – this can be because having a catheter is something that can increase susceptibility to infection, or being unable to fully empty the bladder can also increase the risk.
My initial symptom was a kidney infection – it sent me in to full retention. When it was treated the symptoms appeared to resolve, though it’s likely that I was in partial retention. I then went back into full retention again, and so this, along with increased pelvic pain, were my initial symptoms.
How is it diagnosed?
Fowler’s Syndrome is a difficult condition to diagnose, but the gold standard test is a specialist one called ‘concentric needle electromyography’ (an EMG). Abnormal electrical activity on this test signifies Fowler’s. It’s a pretty uncomfortable test as a needle is used to record from the sphincter.
Other tests that can be carried out include looking at flow rate, residual bladder volume scanning, urethral pressure profile, and ultrasound sphincter volume. However, these tests depend on whether you pass urine naturally or not.
Urodynamics are often the first test that is given as it is commonly carried out in urology departments – if you are in full retention it is unlikely that there will be any useful results, although it can show whether or not your detrusor muscle (the main bladder muscle) is functioning at all.
How long did it take for you to get a diagnosis? Are there any common misdiagnoses?
I was incredibly lucky to get my diagnosis within 4 months of the initial onset of symptoms. On average it takes people seeing 8 professionals before diagnosis and it can take years before a solid treatment plan is given.
The most commonly given first diagnosis is Detrusor Failure (Acontractile Detrusor) as this is a diagnosis that can be given after urodynamics which is the go to test for urological problems. However, when the EMG is done this then highlights the problem with the sphincter muscle and allows the diagnosis of Fowler’s to be given.
When it was first mentioned to you as a diagnosis/given as a preliminary diagnosis how did that make you feel?
In all honesty, I didn’t know what to think. I’d never heard of Fowler’s so it was a lot to get my head around. I didn’t know what to expect, I thought I’d need a catheter for a matter of weeks or months, and certainly didn’t expect to still have one 6 years later! But it was also a relief. No one was telling me that I was making it up or that they didn’t know why my symptoms had started, they could say ‘we might not know a lot, but we do know this’ and that felt reassuring at a time when I didn’t know what to expect next.
What treatments are there? What have you tried in the past? Are there any treatment options you hope to try in the future?
There isn’t a cure for Fowler’s but there are treatments that can be tried. Treatments are still being researched and developed.
The one that a lot of Fowler’s patients try is Sacral Nerve Stimulation – this is particularly good for patients who are in full retention. Those in partial retention may benefit, but their symptoms are more likely to respond to self-catheterisation in order to fully empty the bladder. SNS is the only treatment that has been shown to restore voiding in patients who are otherwise in full retention. In short, SNS is like having a pacemaker for your bladder – it sends electrical signals to your sacral nerves (the nerves that control the bladder). You usually have a trial first to see if it is effective enough and if it is then the full device is implanted.
A Suprapubic Catheter (SPC) is a surgical catheter that is inserted into the bladder through your lower abdomen. This can be better for those with Fowler’s as they bypass the urethra and so there are often fewer urethral spasms when a SPC is in situ rather than a urethral catheter.
Bladder botox has been used for years for people with overactive bladders. It has been used for Fowler’s patients and has shown improvements in bladder emptying for some, as well as reducing bothersome symptoms like spasms and pain. The botox is injected directly into the sphincter and is usually effective for between 3-9 months.
There are two more drastic options as well:
Mitrofanoff surgery is a form of urinary diversion. The purpose of this is to form a man-made channel between the bladder and abdominal wall to allow intermittent self-catheterisation through the abdomen rather than urethrally. Often, it is made using the appendix, but when this isn’t possible part of either the small or large bowel can be used. This option means that you don’t need to have a catheter permanently in place or be attached to a bag.
A Urostomy is a type of stoma and is another form of urinary diversion. A small section of bowel is used to form the stoma and this is connected to the ureters (the tubes that are connected to the kidneys). You then have a stoma bag that collects the urine and needs to be emptied throughout the day and changed regularly.
Both of these are options that are seen as a last resort due to the complexity of them and the recovery time that is needed.
I currently have a SPC (I’ve had it for 4 years now!) and have tried SNS but was told the trial wasn’t effective enough. I’m currently waiting to see if I can have another trial through pain management as it was very effective for my pain levels, and I should find out about this at the end of the month. I’ve been told by one consultant that Mitrofanoff or Urostomy surgery is my only option now, but this isn’t something that has been discussed further.
What is one thing you wish people knew about Fowler’s Syndrome?
That it is so much more than not being able to pee! It’s infections, sepsis, pain, leaking catheters, blood, more pain, spasms, medications, repeat hospital appointments, lack of understanding from professionals and those around you. It causes fatigue and can completely turn your life on its head. It’s a lot.
What is the hardest part about having Fowler’s Syndrome?
For me, it’s the catheter. I have very specific reasons why this is difficult – I have C-PTSD and my catheter is a huge trigger for me and so I find it incredibly hard to live with a catheter that causes such difficult emotions and thoughts to come up. I find catheter changes incredibly difficult because of this and it made self-catheterising near on impossible for me.
Have you had any positive experiences with medical professionals about it, and if so, how has that impacted you?
I have! My first urology nurse was incredible. She was very empathetic and understanding, and I really felt listened to by her. She is actually the reason I started sharing my journey more openly. I had spoken to her about how I felt like I must be the only person in the world my age to be experiencing symptoms like I was, and she sat me down and told me that it was so much more common than people thought. She said she’d love there to be a young urology ‘poster-girl’ (as most leaflets I got given featured pictures of old people on them) and it was after that appointment that I decided to open up more and raise as much awareness as possible.
I’ve also been really lucky to have some incredibly district nurses coming out to me for catheter changes. They’ve held my hand, reassured me when I’ve had flashbacks, stayed at my flat for far longer than they should in order to make sure that I’m ok after a change. They’ve had cups of tea with me and listened to me play the piano, told me about their lives – treated me like a human and not a number. They’ve let me get to know them as much as possible so that I really feel like I have trusted relationships with them, which due to past trauma is something that means a huge amount for me.
If you could change just one aspect of Fowler’s Syndrome, what would it be?
The pain. Definitely the pain. I think I could come to terms with the catheter if I didn’t have to put up with such debilitating pain and spasms.
If you could speak to med students, what is the most important thing you would want them to take away from the conversation?
I actually spoke to some med students about Fowler’s last year! I was an inpatient on a psych ward (so I doubt they were expecting me to start talking urology at them) and they asked if they could have a chat with me and listen to my story. I told them that if there was one thing I wanted them to take from our discussion it was to remember what Fowler’s Syndrome is and to share it with fellow med students and lecturers. I appreciate that it is a rare condition, but it has such wide reaching effects and it still deserves attention and awareness.
If anyone ever has any questions about Fowler’s Syndrome or bladder health in general, I’m always open to answering anything you want to know about!
All my love,
Anna x