If there’s one thing you read in its entirety today, please let it be this.
It been 2 year ago now since I knocked on death’s door! I went from being at a farm swap one day, to dying the next. It wasn’t a rare medical condition that brought me from being a healthy woman to a dying one either. It just hit hard, it hit fast and it would turn my life upside down.
In August of 2022 I had sepsis. And then in October of 2023 it came back. The goal of 2024 is to not get sepsis!
Before I had sepsis, I knew that sepsis was your body’s reaction to infection. I just thought old people got it or those with poor health. I didn’t know people like me(or that even my children) could get it so quickly and I didn’t know that sepsis had long term health affects. I was pretty uneducated about what sepsis was.
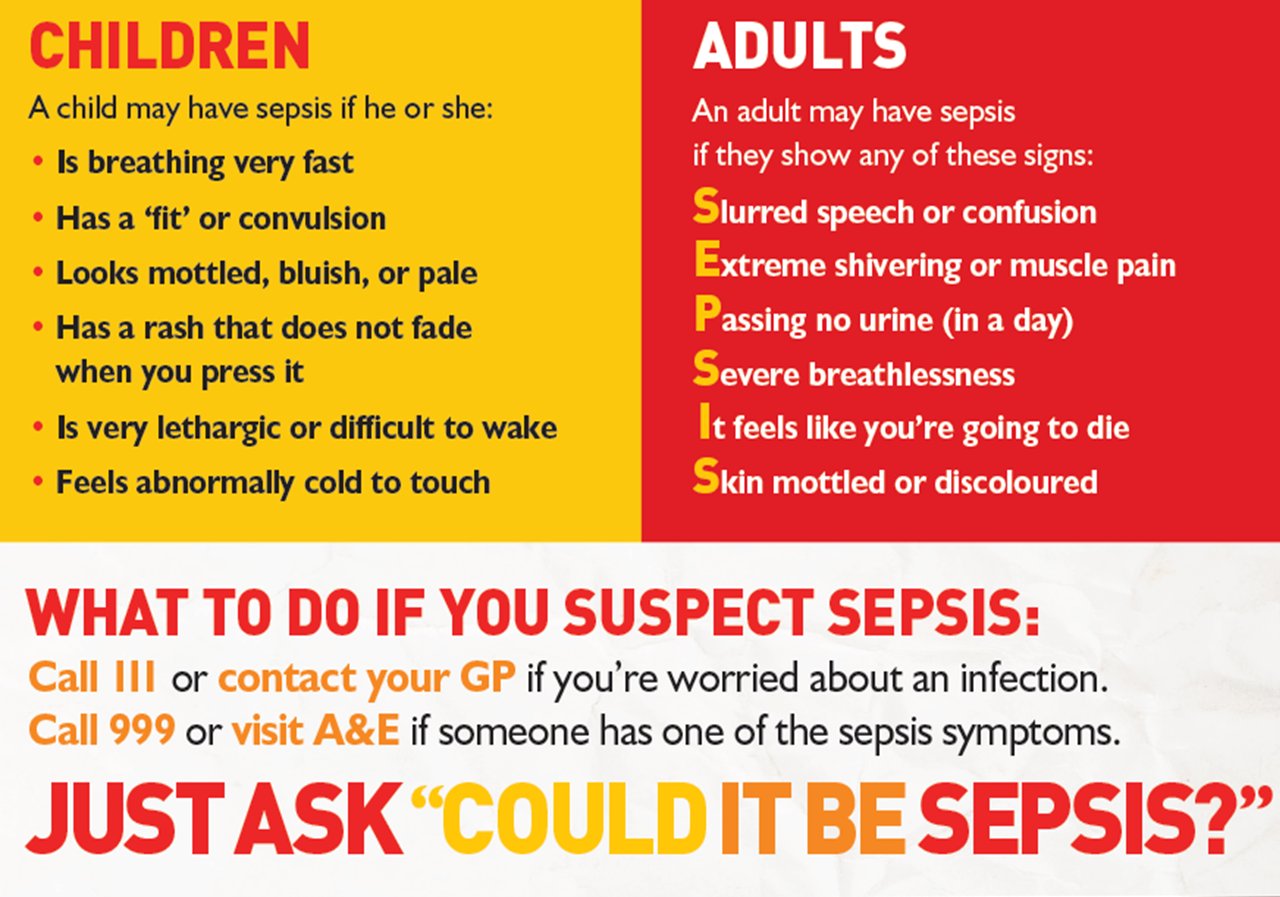
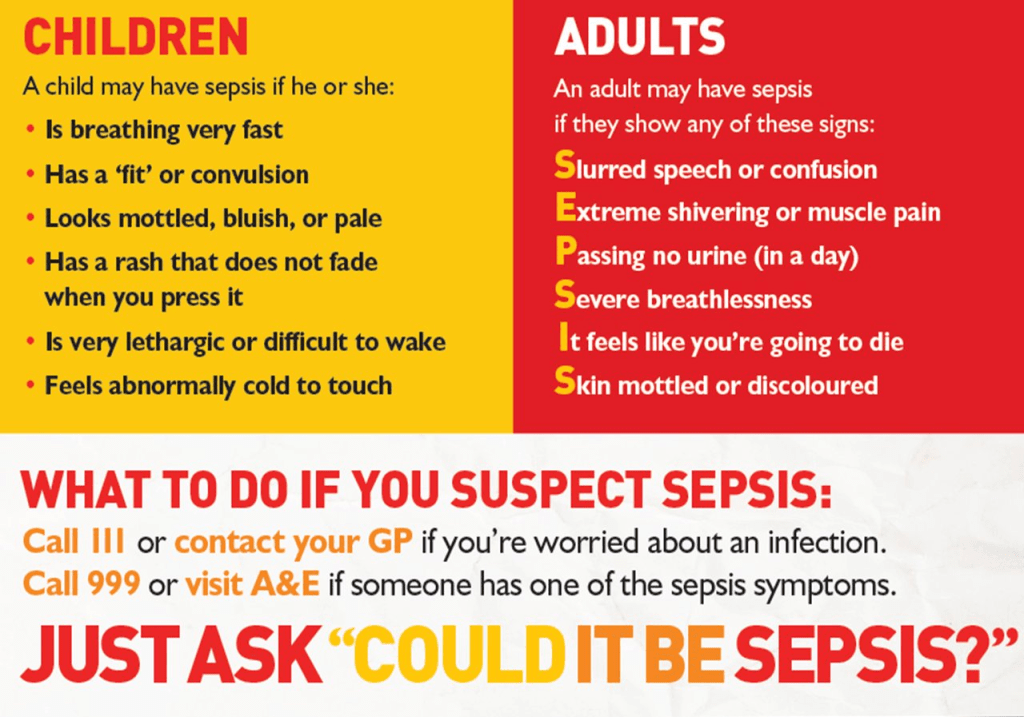
And so it’s become important to me to share what sepsis is, to tell you how to recognize signs of it and to tell you what post-sepsis syndrome is, in hopes that if you are sick you don’t wait to seek medical attention.
Sepsis is the body’s extreme response to an infection. If you don’t get treatment for it, it can lead to organ failure, tissue damage and death.
Symptoms of sepsis are not specific. They can vary from person to person. Initially my blood pressure was low and I had change in mental clarity… my mental state was the most drastic actually. So much so that the hospital ER staff believed I was high on narcotics and was treating me as such. It wasn’t until the hospital made contact with my husband and my best friend arrived at the ER that they were able to ensure the hospital I wasn’t a drug addict and that something else was wrong. And it was! I was finally given a urine drug screen and passed, but the long wait in the ER and being treated as just another addict had delayed much needed treatment and my sepsis turned into septic shock. My best friend saved my life that day.
I spiraled quickly… my blood pressure was low, my respiratory rates were high, I had a fever, I was hallucinating, I was shivering, I lost control of my bladder functions, I felt nauseous. I felt absolutely horrible.
Having sepsis led to my long admittance to the hospital. If I had stayed home, I wouldn’t have made it. If the hospital had delayed longer, I wouldn’t have made it. When people don’t get treatment, sepsis is a leading cause of death. Sepsis ranks higher than breast cancer, lung cancer, and heart attacks. It’s serious stuff. Sepsis can kill an affected person in as little as 12 hours and now that I’ve “been there, done that”, I can testify that this is absolutely true. I was feeling pretty deathly pretty rapidly.
Sepsis is treated with a strict antibiotic regimen. The underlying cause of sepsis or the original infection isn’t always known. It wasn’t ever clearly determined what caused me to get sick. They just have theories.
When I was discharged from the hospital I left knowing I’d be out of work for a bit, taking time to feel better, get rested, etc. But as the days grew to weeks, I wasn’t getting better. I found myself lost(literally), easily confused, at a loss for words, extremely tired, and unable to do tasks I once could. I would wake up and be disoriented to where I was. I’d sit in the house and not know what I was supposed to be doing. I’d try to do simple tasks like pickup dinner at the store and then completely forget why I was there. I would see people and they would act like we knew each other but I had no memory of them. Jason would tell me who they were but it’s like they never existed. I’d relearn people, names, and events. I would later find out that I had post-sepsis syndrome.
Post-sepsis syndrome affects 50% of sepsis survivors. Symptoms vary from psychological to physical effects. My short term memory was heavily impacted as was my cognitive functioning, similar to that of a traumatic brain injury. I had extreme fatigue and chest pains. My once normal heart now had tachycardia.
Post sepsis has required me to take medications just to stay awake during the day and to stimulate my brain. It’s changed my heart functioning and I take medications to keep it beating the right way. It’s made me forget some moments I desperately want to remember. It’s made simple memory tasks into harder ones. It’s made me rely on others to help do tasks I once could easily do. It’s enrolled me in rehab where we practiced skills to help my injured brain.
Now I do things on my speed and with tons of support from my husband and kids.
If you say “wow! I didn’t know!” It’s because I have the best support system someone could ask for. You don’t see me fail because of them. I succeed because they are behind me filling in the gaps.
I don’t share this because I want prayers or good vibes. I don’t want sympathy. On my two year almost dying anniversary, I want you to take sepsis seriously. Very seriously. I want you to go the doctor when you have an infection. I want you to take 5 mins today and to Google sepsis and read about all the signs and symptoms of sepsis.
I want you to be healthy. ![]()